WHAT IS OSA?
Obstructive sleep apnea (OSA) is a sleep-related breathing disorder in which your breathing can be ceased for more than 10 seconds as long as even 100 to 120 seconds, repeatedly during the night while sleeping. This can lead to a drop in blood oxygen level, increased CO2 retention, the release of stress hormone- cortisol[1], and frequent arousals with loud snoring and
choking sensation. This results in disturbed sleep, excessive daytime sleepiness, tiredness, concentration problems, and mood change issues.
In a long run, this can even cause other major issues like increased chances of heart disease, stroke, memory loss, hypertension, diabetes, and even depression.[2]
ENT Evaluation in OSA
Various anatomical and pathophysiological factors are associated with the cause of OSA, which can determine the course of action for the treatment a little more complex. An ENT (eyes, nose, throat) specialist (Otorhinolaryngologist) can examine the upper airway to find out in detail what is causing that obstruction. [3]
[1] “Stress and Sleep Apnea.”
[2] “Osa Aasm – Google Search.”
[3] “Sleep Apnea Treatment by ENT.”
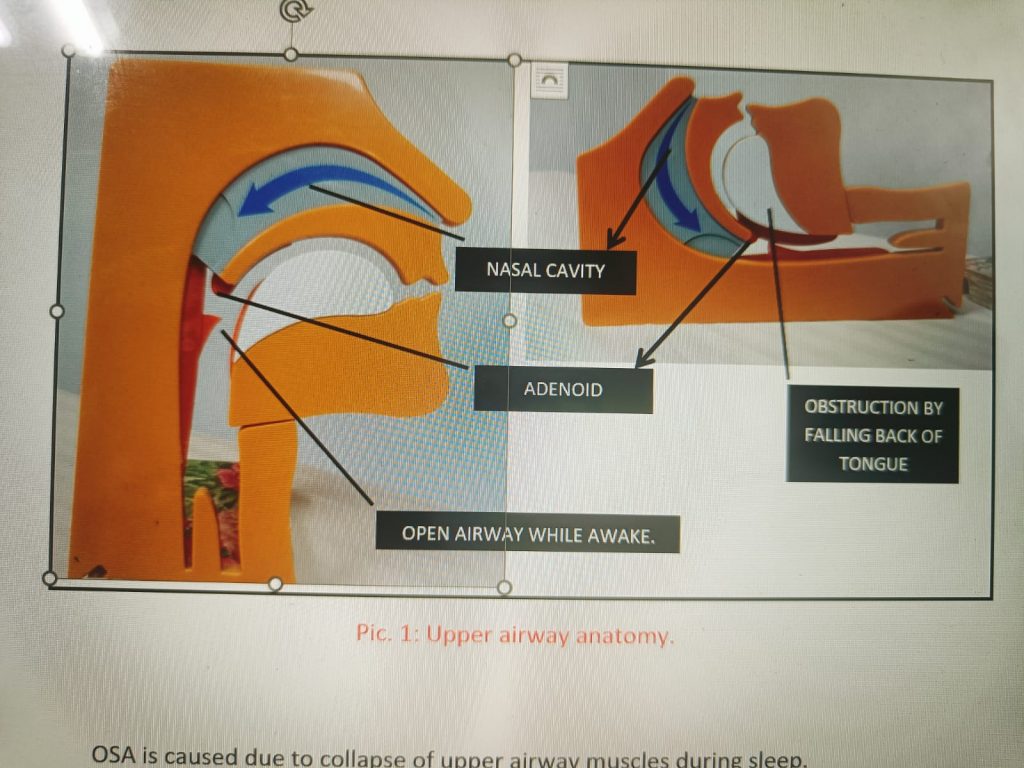
OSA is caused due to collapse of upper airway muscles during sleep.
Certain ENT disorders that may lead to OSA are:
- Obstructed nasal airways: in cases of nasal polyps or inferior turbinate hypertrophy.
- Deformities of the nose or nasal septa, such as the deviated septum, double septum, and septal hematoma can cause an obstruction.
- Inflammatory conditions of the nose: cold, chronic rhinosinusitis, or allergic rhinitis.
- Long soft palate and/or uvula
- Excessive bulkiness of throat tissue: Children with large tonsils and adenoids often snore.
- Overweight people have bulky neck tissue.
- Cysts or tumors can also cause bulk which may cause snoring.
The ENT causes are relatively simple conditions that can be treated by safe and simple medical and/or surgical procedures.
OPTIONS FOR THE TREATMENT OF OSA.
There are various treatment options for sleep apnea which can be majorly divided into non-invasive and invasive adjuncts.[1]
- NON-INVASIVE– The gold standard treatment for OSA that can be recommended for all the patients with moderate to severe apnea regardless of their anatomical differences in the upper airway causing OSA, is PAP (Positive Airway Pressure) therapy. More than a treatment, it is a control therapy to keep the airway open during sleep and can hence help in providing uninterrupted good quality sleep. With the correct fit and comfort of mask and straps, adherence and good compliance to the PAP (CPAP/BIPAP) can enhance your overall sleep quality.
- EXERCISES and DIET CONTROL- Weight reduction exercises and some oropharyngeal exercises to tone the muscles of the upper airway like the soft palate, throat, and tongue which can help the patients reduce the severity of OSA. However, a complete cure of the issue is only possible in mild OSA patients (AHI 5-15).
- ORAL APPLIANCES (MADs) (mandibular advancement devices)- These are specially designed mouthpieces to bring forward the jaw to facilitate the opening of the airway. Some hold the tongue in place hence avoiding closure of the airway by falling back of the tongue.
- UPPER AIRWAY STIMULATION- It’s a small electrical device placed in the chest just like a pacemaker, below the skin and above the ribs. It has an electrode that is connected to the nerve which controls tongue muscles by stimulating it during sleep and thus keeping the airway open.
- SWITCHING POSITIONS- Some of you may have sleep apnea and snoring by sleeping in a supine (lying on the back) position. Switching position from supine to either side may benefit you.
- SURGERY- The last resort is SURGERY – Uvulopalatopharyngoplasty (UPPP) -Surgeons remove the soft tissue from the back of your palate and may take out your tonsils and uvula (the soft tissue that hangs down the back of your throat). Other surgeries may involve your jawbones, other soft tissue, or your nose.
WHICH OSA PATIENTS SHOULD BE REFERRED FOR SURGERIES?
(1) Patients who are intolerant or unaccepting of PAP therapy, BMI <40 kg/m2.
(2) Clinicians discuss referral to a bariatric surgeon with adults with OSA and obesity (class II/III, BMI ≥ 35) who are intolerant or unaccepting of PAP as part of a patient-oriented discussion of alternative treatment options (STRONG).
(3) Adults with OSA, BMI < 40 kg/m2, and persistent inadequate PAP adherence due to pressure-related side effects as part of a patient-oriented discussion of adjunctive or alternative treatment options (CONDITIONAL).
(4) Patients with obvious upper airway anatomic abnormalities are potentially amenable to surgery as initial OSA treatment.
WHICH SURGERIES ARE PERFORMED FOR OSA?
Surgical treatment may involve various procedures that are performed in different stages depending on the patient’s sites of obstruction.[2]
Different sites for obstructions are nasal, nasopharyngeal, oropharyngeal, hypopharyngeal/retrolingual, or a combination of these.
PROCEDURES:
- Nasal reconstruction: Removal of nasal polyps or turbinates, or straightening of a deviated nasal septum.
This may increase airflow through the nose though it does not completely cure (OSA). It may improve daytime and nighttime breathing through the nose and may enable better use of a positive airway pressure device.
- Uvulopalatopharyngoplasty (UPPP): This is the most common operation which widens the airway behind the tongue by removing excess tissue from the sides of the throat behind the tongue, shortening the soft palate, and removing the uvula.
It requires hospitalization and recovery may take several weeks.
2 variants of the operations can be performed
- With a laser (laser-assisted uvulopharyngoplasty, or LAUP)
- By a radiofrequency probe (somnoplasty).
Although snoring is frequently improved with these operations, only approximately 40% of persons undergoing UPPP have resolution or major improvement in their OSA. Furthermore, it is unclear whether the success rates from LAUP or somnoplasty are comparable to those for UPPP.
- Mandibular osteotomy with genioglossus advancement prevents posterior collapse during sleep.
- Hyoid myotomy and suspension. In this hyoid bone and its muscle attachments to the tongue and airway are pulled forward with the aim of increasing airway size and improving airway stability in the retrolingual and hypopharyngeal airway (airway behind and below the base of tongue).
- In more severe cases, maxillomandibular advancement (MMA) with advancement genioplasty may be indicated. In this operation, the upper and lower jaws are surgically fractured, and both are moved forward to enlarge the airway.
- Hypoglossal Nerve Stimulation: The tongue is stimulated by the hypoglossal nerve which has an electrode that is stimulated by sensing electrodes placed on the chest wall. This moves the tongue forward thereby preventing the collapse of the tongue backward and avoiding obstruction of the airway.[3]
HOW EFFECTIVE IS THE SURGERY OVER CPAP THERAPY?
Even after appropriate surgery, sleep apnea may persist along with symptoms.
The success of surgery in OSA is generally measured by achieving
- RDI of less than 5,
- Improvement of oxygen least to 90 percent or more with no desaturations below 90 percent and
- Quality of life improvements with elimination or significant reduction of OSA symptoms.
Weight loss and maintenance of healthy life is an extremely difficult goal to be achieved with your cooperation and dedication, without which all the measures can be a huge failure.
Sleep apnea surgery risks and potential complications include:
- Allergic reactions to anesthesia.
- Bad breath
- Blood clots
- Breathing problems
- Death (rare complication following UPPP)
- Excessive bleeding
- Fever
- Nausea
- Pain
- Persistent throat dryness
- Recurrence of obstructive sleep apnea or development of central sleep apnea
- Snoring
- Skeletal collapse
- Swelling around the surgery site
- Temporary numbness
- Tongue dysfunction or weakness
- Urinary retention
- Vomiting
Complications differ on the type of surgery.
Another important thing to be minded is that people with sleep apnea are higher risk surgery patients because anesthesia relaxes throat muscles and increases the risk of airway collapse.
TO CONCLUDE SURGERY VS CPAP FOR TREATMENT OF OSA-
It may be stated that OSA is not a simple but a chronic multifactorial disorder that requires lifelong follow-ups and monitoring and has patient-oriented treatment plans. Though surgery can be a tempting option for the patient, the success rate of reversal of OSA is sparse. Adherence to the CPAP compliance can be a boon for the increased lifespan of a patient with OSA. Hence, the decision to take up an invasive surgery should be made only by the surgeon, if the compliance of the CPAP is poor or the patient can be easily reversed by surgery if the site of obstruction is known and can be corrected.[4]
BIBLIOGRAPHY:
- Carvalho, Bettina, Jennifer Hsia, and Robson Capasso. “Surgical Therapy of Obstructive Sleep Apnea: A Review.” Neurotherapeutics 9, no. 4 (October 2012): 710–16. https://doi.org/10.1007/s13311-012-0141-x.
- Ephros, Hillel D., Mansoor Madani, and Sumitra C. Yalamanchili. “Surgical Treatment of Snoring & Obstructive Sleep Apnoea.” The Indian Journal of Medical Research 131 (February 2010): 267–76.
- “Osa Aasm – Google Search.” Accessed March 21, 2022. https://www.google.com/search?q=osa+aasm&oq=osa+aasm&aqs=chrome..69i57j0i22i30l3j0i390l2.3917j0j15&sourceid=chrome&ie=UTF-8.
- “Sleep Apnea Treatment by ENT.” Accessed May 17, 2022. https://mountainent.com/blog/sleep-apnea-treatment-by-ent.
- WebMD. “Sleep Apnea Treatment Options.” Accessed May 19, 2022. https://www.webmd.com/sleep-disorders/sleep-apnea/ss/slideshow-sleep-apnea-treatment-options.
- WebMD. “Stress and Sleep Apnea: Is There a Link?” Accessed May 17, 2022. https://www.webmd.com/connect-to-care/sleep-apnea/is-there-a-link-between-sleep-apnea-and-stress.
- “Surgical Treatments | Sleep Apnea.” Accessed May 20, 2022. https://healthysleep.med.harvard.edu/sleep-apnea/treating-osa/surgical.
[1] “Sleep Apnea Treatment Options.”
[2] Ephros, Madani, and Yalamanchili, “Surgical Treatment of Snoring & Obstructive Sleep Apnoea.”
[3] “Surgical Treatments | Sleep Apnea.”
[4] Carvalho, Hsia, and Capasso, “Surgical Therapy of Obstructive Sleep Apnea.”
